1801006143 - long
1801006143 - long case
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
A 57 year old male, resident of Nakrekal, mason by occupation came to hospital with chiefs complaints of
shortness of breath since 1 week
Decreased urine output since 1 week
HISTORY OF PRESENT ILLNESS
patient was apparently asymptomatic 1 week back then he had shortness of breath while walking upstairs and walking at normal pace (grade 2) which gradually progressed to shortness of breath at rest in last 1 week ( grade 4). Shortness of breath aggravate by doing work and on lying horizontally on bed. Relieved by taking rest in reclined position
There is history of gradual decreased urine output since 1 week, narrow stream lime urine
No H/O fever, chronic cough, weight loss, hemoptysis, sputum
No H/O chest pain, sweating, palpitations, syncope
No H/O burning micturition, difficulty in micturition
DAILY ROUTINE :
He wakes up around 5 am in the morning and does his household chores , goes to work for 5 to 6 hrs and returns back home around lunch time 1pm and take rest for the day. He will have his dinner around 7 30 pm and goes to sleep at 9 pm. He now has stopped his daily work since a year.
PAST HISTORY
No similar complaints iyn past
History of pedal edema on and off since 1 year, present upto level of ankle
He is a known case of hypertension since 1 year and he takes telmesartan 40mg every day morning after breakfast
No H/O diabetes, asthma, tuberculosis, epilepsy
PERSONAL
Appetite: normal
Sleep: adequate
Bowel habits : regulary
bladder habits : decreased urine output
Addictions: he used to drink 90 ml alcohol and smoke 5 to 6 BD’s regularly since last 30 to 35 years. Since last 1 year he only drink and xwwsmoke occasionally
FAMILY HISTORY
No similar complaints in family
TREATMENT HISTORY
Since last 4 years he is taking analgesics for knee pains. He took them occasionallyz²q211 in the beginning , but since last 2 years he took them daily or on alternate days.
Since last 1 year he is taking telmesartan 40 mg every day morning for hypertension
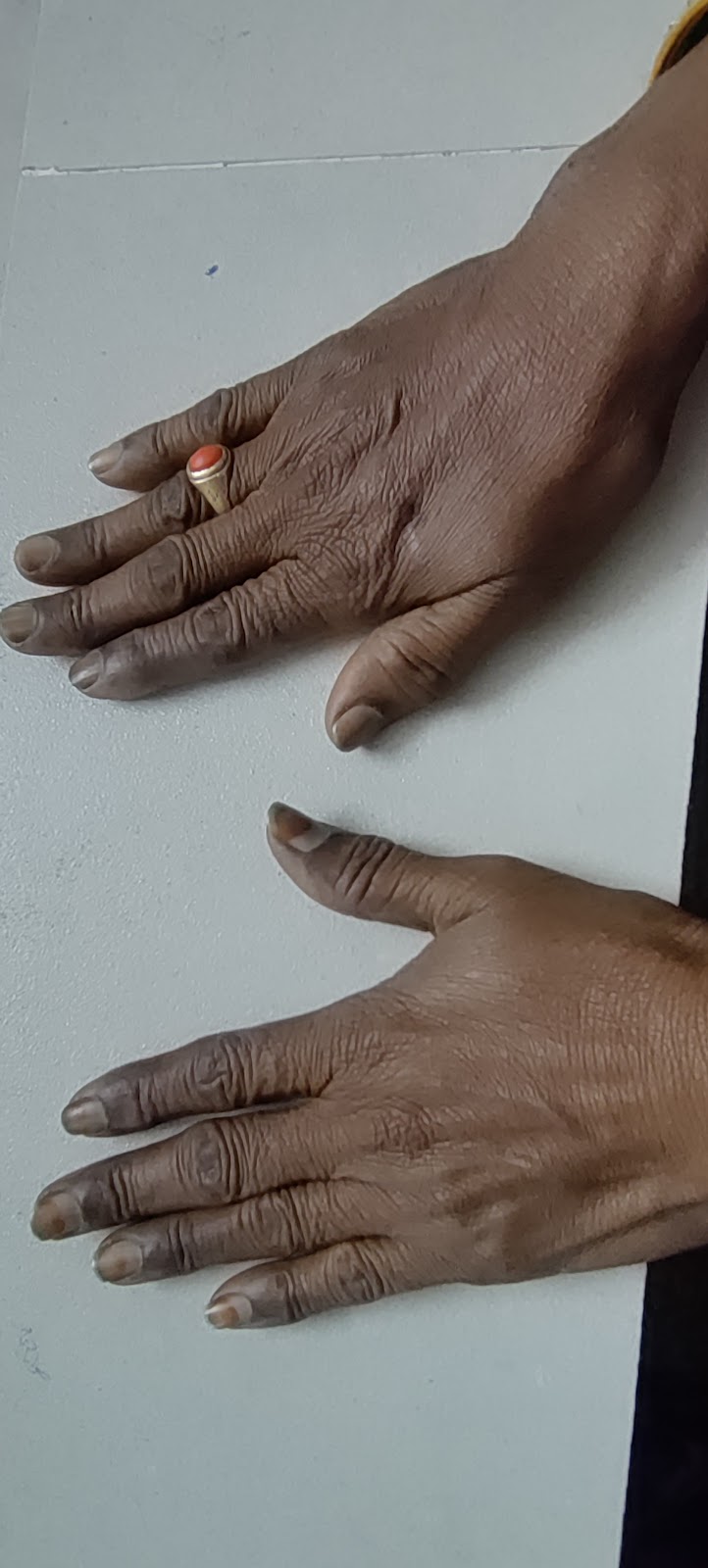
GENERAL EXAMINATION
pallor - absent
Icterus - absent
Clubbing - absent
Cyanosis - negative
Lymphadenopathy - negative
Generalised edema - negative
VITALS
Temperature: afebrile
Pulse rate: 90 bpm
Respiratory rate: 18 cpm
Blood pressure: 130/80 mm hg
GRBS : 124 mg/dl
SpO2 : 92 %
SYSTEMIC EXAMINATION
Respiratory system
Inspection:
Trachea is in midline
Shape of chest - elliptical
Chest is bilaterally symmetrical
No chest wall defects
There is a scar of approximately 2 to 3 cm on the right side of front of the chest. Similarly — Lesions are present on the back of the chest
Palpation:
Trachea is central on palpation
No intercostal widening/crowding, subcutaneous emphysema, intercostal tenderness
Chest movements are bilaterally symmetrical
Chest measurements: 34 cm
Tactical vocal fremitus
Right Left
Supraclavicular R R
Infraclavicular R R
Mammary R R
Inframammary R R
Axillary R R
Infra axillary R R
Supra scapular R R
Infra scapular R R
Inter scapular R R
(R - resonant)
Auscultation:
Left Right
Supraclavicular
Nvbs. Nvbs
Infraclavicular
Nvbs. Nvbs
Mammary
Nvbs. Nvbs
Inframmamry
Wheeze. Nvbs
Axillary
Nvbs. Nvbs
Infra axillary
Wheeze. Nvbs
Suprascapular
Nvbs. Nvbs
Infrascapular
Nvbs. Nvbs
Interscapular
Nvbs. Nvbs
(Nvbs - Normal vesicular breath sounds )
Wheeze is audible in right and left inframammary area
CVS
Inspection:
Chest wall is normal in shape and is bilaterally symmetrical
Apical impulse not well appreciated
Mild rise in jvp
No precordial bulge, kyphoscoliosis
No visible veins and sinuses
Palpation:
Apex beat is felt at 6th intercostal space lateral to mid clavicular line
All peripheral pulses are felt and compared with opposite side
No parasternal heaves, precordial thrills
Percussion:
Left heart border is shifted laterally, and right heart border is present retrosternally
Auscultation:
Mitral, tricuspid, pulmonary, aortic and Erb’s area auscultated
S1 S2 are heard, no abnormal heart sounds
CNS
Higher mental functions are intact
Cranial nerve functions are intact on right and left sides
Motor system: bulk and tone are normal
Power is 5/5 in all 4 limbs
Deep tendon reflexes are present and normal
Superficial reflexes are present and normal
No involuntary movements
No signs of cerebellum dysfunction
No neck stiffness, kernigs and Brudzinski’s signs are negative
ABDOMINAL EXAMINATION
Inspection:
Abdomen is flat and flanks are free
Umbilicus is inverted
No visible scars, sinuses, dilated veins, visible pulsation
Hernial orifices are normal
Palpation:
No local rise of temperature
No tenderness and enlargement of Liver, spleen, kidney
Percussion:
No fluid thrill
Liver span is normal, no spleenomegaly
Auscultation:
Bowel sounds are heard
Provisional diagnosis: heart failure with hypertension
INVESTIGATIONS
Hemoglobin - 7.7 gm/dl
Total count - 14,100 cells/cumm
Lymphocytes - 16%
PCV - 23.1 vol%
SMEAR :
WBC - increased count (neutrophilic leucocytosis)
RBC- normocytic normochromic
Platelets - adequate
Serum creatinine - 4.0 mg/dl
Blood urea - 95mg/dl
ABG :
PH 7.43
Pco2 - 31.6 mmHg
Po2 - 64.0 mmHg
HCO3 - 21.1 mmol/l
Urine examination :
albumin ++
sugar nil
pus cells 2-3
epithelial cells 2-3
Red blood cells 4-5
Random blood sugar - 124 mg/dl
ECG:
2D echo:
DIAGNOSIS
Heart failure with reduced ejection fraction
Chronic kidney disease on maintenance dialysis
TREATMENT
Inj. Thiamine 100mg IV/TID
Inj. Lasix 40 mg/IV/BD
Inj. Erythropoietin 4000 IU/SC/ once weekly
Inj, PAN 40mg/IV/OD
Inj piptaz 2.25 gm IV/TID
Tab. Nicardia retard 10 mg/RT/BD
Tab. Metoprolol 12.5 mg/RT/OD
Cap. Bio D3 retard od
Hemodialysis
Nebulisation with duolin 8th hourly & budecort 12th hrly
Intermittent CPAP
regular monitoring of vitals







Comments
Post a Comment