A 53 year old male came with the c/o fever, facial puffiness ,yellowish discoloration of eye
This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CHEIF COMPLAINTS
c/o-fever days, facial puffiness since 6 days
C/o yellowish discoloration of eye since 1 day
HISTORY OF PRESENT ILLNESS:
patient was apparently asymptomatic 6 days ago then developed fever, insidious onset, high grade, on and off at night times.
Facial puffiness more in morning gradually improves.
clo-yellowish discoloration of eye.
H/o- Increased urine output since 6 days
H/o dry cough since 6 days
No H/O chest pain abdominal pain, abdominal distension,pedal edema
No H/o burning micturition
No H/O loose stool, vomiting
PAST HISTORY:
k/c/o. Type II Dm since 1 year
On medication T. METFORMIN 500mg , T-GLIMIPERIDE 2mg.
HTN since 3 years on unknown medication.
Not a k/c/o - Epilepsy, thyroid disorder, Asthma, TB, CAD,CVA.
PERSONAL HISTORY:
Diet: Mixed
Appetite: Normal
Sleep: Normal
Bowel and bladder movements: Regular
No addictions.
GENERAL EXAMINATION:
Patient is conscious, coherent, cooperative and well oriented to time, place and person.
Moderately built and nourished.
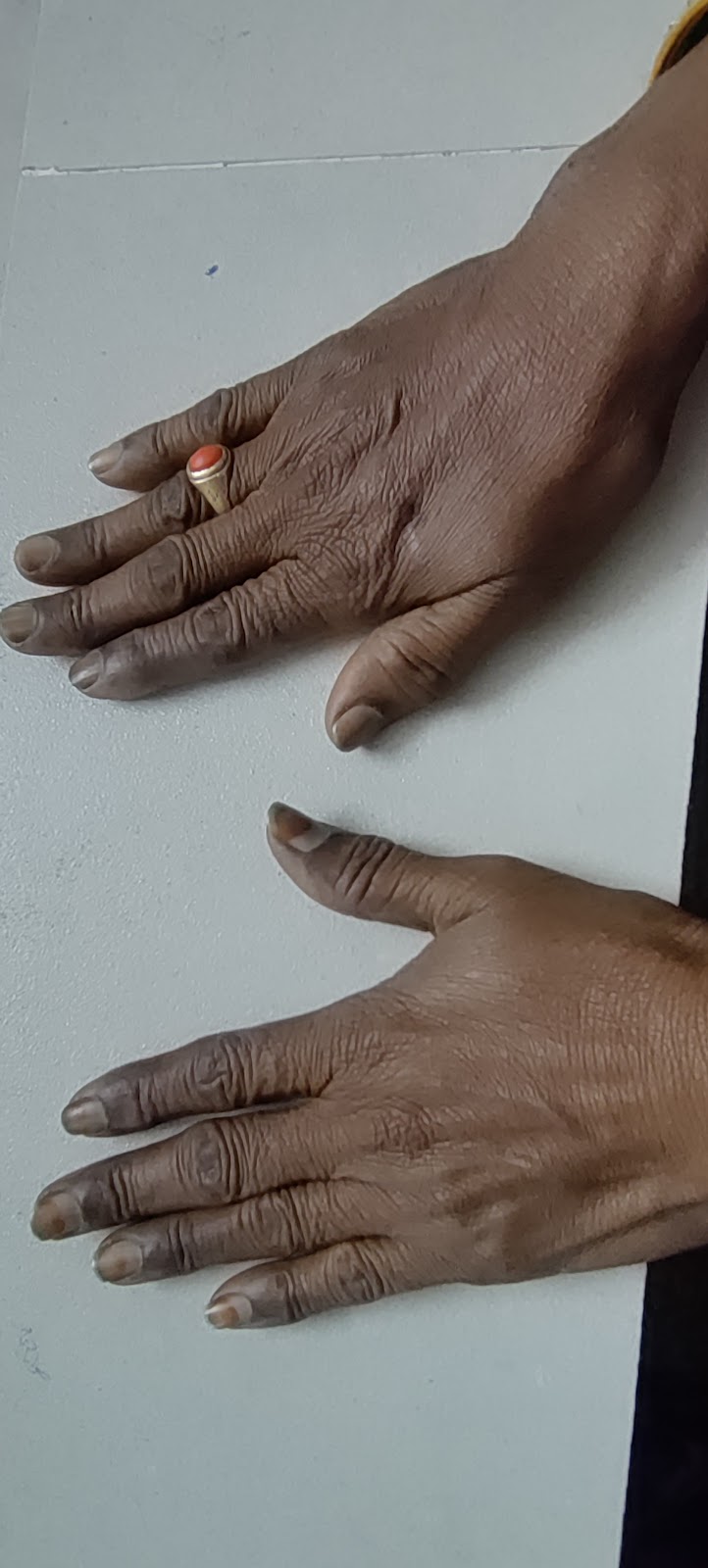
pallor + , icterus +
No cyanosis, clubbing, lymphadenopathy, pedal edema.
VITALS:
Temp:98.4F
PR: 98 bpm
BP: 110/70mm hg
RR:19cpm
SPO2: 98%
Systemic examination:
CVS: s1, s2 heard ,no murmurs.
R/S:
Inspection:
Chest bilaterally symmetrical,
Shape- elliptical
Trachea- Central
Palpation:
Trachea is Central
Normal chest movements
Vocal fremitus is normal in all areas
Percussion: in sitting postion
Rt. Lt
Supraclavicular. N(resonant). N
Infraclavicular. N N
Mammary region. N. N
Inframammary region. N. N
Axillary region. N. N
Infra axillary region. N. N
Supra scapular region. N. N
Interscapular region. N. N.
Infrascapular region. N. N
Auscultation:
Normal vesicular breath sounds
No added sounds
Vocal resonance is normal in all areas.
CNS:
Higher motor functions - intact
Cranial nerves - intact
Motor system:
Rt- UL. LL. Lt- UL. LL
Bulk - N N. N. N
Tone - N. N. N. N
Power - 5/5. 5/5. 5/5. 5/5
Reflexes:
UL LL
Biceps. 2+. 2+
Triceps. 2+. 2+
Supinator. 2+. 2+
Knee. 2+. 2+
Ankle. 2+. 2+
Sensory system: intact
Co ordination is present
P/A :soft, non tender
Clinically spleen and liver not palpable
USG abdomen:
TREATMENT:
INJ FALCIGO 120 mg IV
INJ NEOMOL IV / SOS
INJ VITCOFOL 1ml /1500mcg/IM
T. TELMA 40 mg
T. GLIMI-M2
T. DOLO 650 mg
T.TUSQ
































Comments
Post a Comment