80YEAR OLD MALE WITH FEVER AND BURNING MICTURATION
A 80 year old male patient came with
Chief complaints :
Fever since 20 days
Weakness of both lower limbs since 15 days
Pain in Rt. lower quadrant of abdomen since 10 days
Decreased urine output since 5 days
Burning sensation while passing urine since 5 days
HOPI :
Patient was apparently asymptomatic 20 days back, then he developed fever since 20 days which is high grade, associated with chills and rigors, no diurnal variation, relieved with medication. He visited the local RMP for the same and got a CUE done and was told by the RMP that he had urine infection. He had weakness of both lower limbs since 15 days(unable to stand and walk on his own). Then, he had pain abdomen in the right lower quadrant of abdomen and in the lower back which had no aggravating and relieving factors. He also had decreased urine output and burning sensation while passing urine since 5 days.
Shortness of Breath present (on and off)
No h/o chest pain
No h/o headache.
Past History :
Patient is a k/c/o Asthma and is not on medication
K/c/o Hypertension since 10 years and is on Amlodipine 5 mg once daily.
H/o renal calculi 10 years back.
K/c/o BPH 10 years back
Hospital admission for 15 days for Decreased urine output and abdominal distension 10 years back. Was told that the Creatinine was raised. Underwent treatment for 6 months.
Decreased hearing since 6 months
Uinary incontinence since 5 years.
Known case of Hepatitis since 10 years.
Not a k/c/o TB, DM, ASTHMA, EPILEPSY
Personal History :
Diet : mixed
Appetite : Decreased
Sleep : Disturbed
Bowel movements : Constipation since 5 days
Bladder movements : Decreased urine output and burning micturition since 5 days
Addictions : Consumes alcohol occasionally
On Examination :
Patient is conscious, coherent and cooperative.
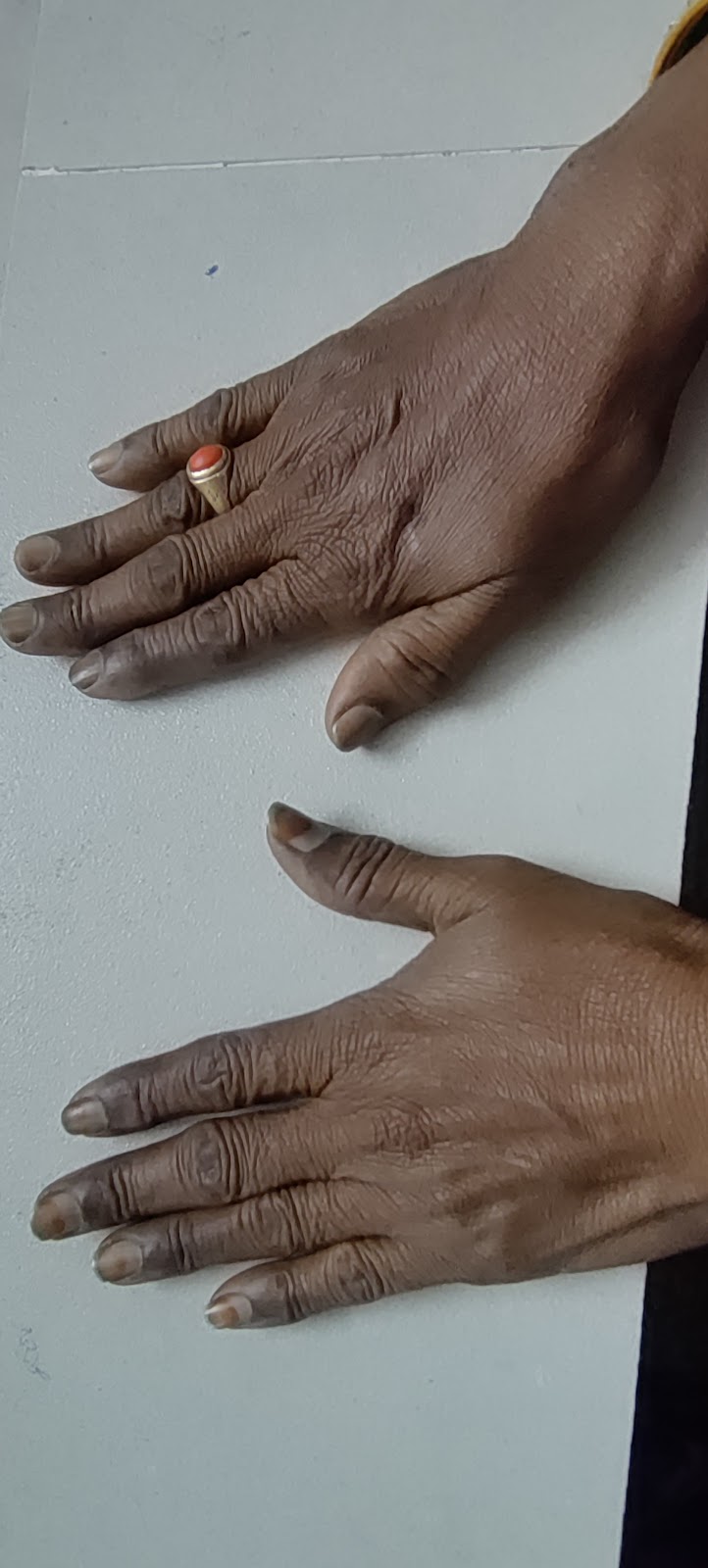
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema .
VITALS :
AT THE TIME OF ADMISSION :
TEMP. : 99.6 F
PR : 80 BPM
RR : 16 CPM
BP : 110/70 MM HG
SpO2 (on Room air) : 98%
GRBS : 106 mg%
On Systemic Examination:
CVS : S1, S2 heard
RS : BAE present
P/A : soft, Non tender
CNS :
HMF Intact
TONE : RIGHT LEFT
UPPER LIMB. N. N
LOWER LIMB. N. N
POWER :. RIGHT. LEFT
UPPER LIMB. 4/5 4/5
LOWER LIMB. 4/5. 4/5
REFLEXES :
BICEPS. +++. +++
TRICEPS +++. +++
SUPINATOR +. +
KNEE. +. -
ANKLE +. -
PLANTAR :. FLEXOR. MUTE
7 am

1 pm
5. ABG (3 PM)
6. REVIEW USG FOR BLADDER VOLUME (PRE VOID AND POST VOID)
7. ECG
8. RFT
9/10/22
1. Hemogram
2. RFT
3. CUE
4. REVIEW USG FOR BLADDER VOLUME (PRE VOID AND POST VOID)

10-10-22
1. Hemogram
2. RFT
3. Urine Culture and Sensitivity
4. Blood Culture and Sensitivity
5. PLBS
6. HbA1C
11-10-22
1. HEMOGRAM
2. RFT
3. FBS
4. 24 hr urinary protein
5. 24 hr urinary creatinine
CROSS CONSULTATION NOTES :
1. UROLOGY REFERRAL
Provisional Diagnosis : UTI
Treatment :
Day 2 :
1. TAB. NITROFURANTOIN 100 MG PO/BD
2. INJ. NEOMOL 1 G/IV/SOS (IF TEMP.>101 F)
3. IV FLUIDS NS @ 75 ML/HR
4. INJ. PIPTAZ IV/OD
5. TAB. DOLO 650 MG PO/TID
6. INJ. PAN 40 MG /IV/OD
7. T. TAMSULOSIN 0.4 MG/PO/HS
8. INJ. ZOFER 4 MG/IV/OD
Proctolytic enema was administered to the patient i/v/o constipation since 5 days
SOAP Notes :
AMC BED 1
Day 3 (9-10-22)
S : Fever spikes present
Pain in groin while walking
Passed stools
O :
Patient is conscious, coherent and co-operative
Temp : 99.1 F
BP : 110/60 mmHg
PR : 80 BPM
RR : 16 CPM
SpO2 : 98%
GRBS : 98 mg/dl
A : URINARY TRACT INFECTION WITH ACUTE KIDNEY INJURY
P :
1. INJ. PIPTAZ 2.25 G/IV/TID
2. T. URIMAX-D 0.4/0.5 MG/PO/OD
3. T. DOLO 650 MG/PO/TID
4. INJ. ZOFER 4 MG/IV/SOS
5. INJ. NEOMOL 1 G/IV/SOS (IF TEMP. >101 F)
6. SYP. CREMAFFIN 10 ML/PO/HS
7. T. AMLONG 5 MG/PO/OD
8. STRICT I/O CHARTING
9. MONITOR VITALS (BP AND TEMP. EVERY 4TH HOURLY)
AMC BED 1
Day 4 (10-10-22)
S : Pain in right loin
O :
Patient is conscious, coherent and co-operative
BP : 130/80 mmHg
PR : 80 BPM
RR : 25 CPM
Temp : 96 F
SpO2 : 95%
GRBS : 92 mg/dl
A : COMPLICATED URINARY TRACT INFECTION WITH ACUTE KIDNEY INJURY
P :
1. INJ. PIPTAZ 2.25 G/IV/TID
2. T. URIMAX-D 0.4/0.5 MG/PO/OD
3. T. DOLO 650 MG/PO/TID
4. INJ. PAN 40 MG/IV/OD
5. INJ. ZOFER 4 MG/IV/SOS
6. INJ. NEOMOL 1 G/IV/SOS (IF TEMP. >101 F)
7. SYP. CREMAFFIN 10 ML/PO/HS
8. T. AMLONG 5 MG/PO/OD
9. IV FLUIDS NS @ 75 ML/HR
10. STRICT I/O CHARTING
11. MONITOR VITALS (BP AND TEMP. EVERY 4TH HOURLY)
MEDICAL WARD
Day 5 (11-10-22)
S : Pain in right loin
O :
Patient is conscious, coherent and co-operative
BP : 130/80 mmHg
PR : 82 BPM
RR : 18 CPM
Temp : 96 F
SpO2 : 97%
GRBS : 105 mg/dl
A : COMPLICATED URINARY TRACT INFECTION WITH ACUTE KIDNEY INJURY
P :
1. INJ. PIPTAZ 2.25 G/IV/TID
2. T. URIMAX-D 0.4/0.5 MG/PO/OD
3. T. DOLO 650 MG/PO/TID
4. INJ. PAN 40 MG/IV/OD
5. INJ. ZOFER 4 MG/IV/SOS
6. INJ. NEOMOL 1 G/IV/SOS (IF TEMP. >101 F)
7. SYP. CREMAFFIN 10 ML/PO/HS
8. T. AMLONG 5 MG/PO/OD
9. T. RENERVE - P PO/HS
10. IV FLUIDS NS @ 75 ML/HR
11. STRICT I/O CHARTING
12. MONITOR VITALS (BP AND TEMP. EVERY 4TH HOURLY)
.





























































Comments
Post a Comment