60 year old male with ckd
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
A 60 year old male presented with
Chief complaints :
Vomiting on and off and
Decreased appetite since 4months
Fever since 3 months on and off
generalized itching 5 days back
History of present illness:
Patient was apparently asymptomatic 6 years back and then he developed joint pains in the great toe and proximal interphalangeal joint and had migrating joint pains and was diagnosed as gout in their regional hospital and was found that creatinine was increased, he used allopathy medication and ayurvedic medication for gout, he was on medication (?)for kidney problem for few years and stopped,
4 months back he developed generalized itching over the body, anorexia, epigastric pain, vomitings which is non billious with food particles in it and he went to regional hospital where he was diagnosed as ckd creatinine (6.2 mg/dl) and underwent 2 sessions of dialysis and
he developed infection
after dialysis (central line induced) and he was admitted in icu for one day and treated,
he had h/o of low grade fever since one month with chills and rigors since one month which is continuous subsided on using medication,
h/o of constipation since many years, dry cough since 2 months, itching subsided after dialysis and recurrent itching episodes were present for which he used medication and it got subsided ,
since one week he is having diarrhea, anorexia, weakness and admitted and he is on medication (?)of ckd since 6 days
And had no h/o of burning mituration and decreased mituration
Day before yesterday he was admitted for dialysis
Past history:
Patient is hypertensive since 7 years not on regular medication
No h/o diabetes, seizures, tb, leprosy.
H/o itching chin area 3 months back and took medication , subsided on medication
3 months back underwent dialysis at khammam private hospital
H/o central line infection since 3 months
PERSONAL HISTORY:
Diet -mixed
Appetiteb - decreased
Sleep -decreased
Bowel - has constipation
Bladder - regular
Addictons - occasional drinks alcohol 90ml
Family history:
father has history of joint pains
Drug history :
no drug allergies and food allergies
GENERAL EXAMINATION:
Patient is conscious, coherent and cooperative. moderately built and nourished.
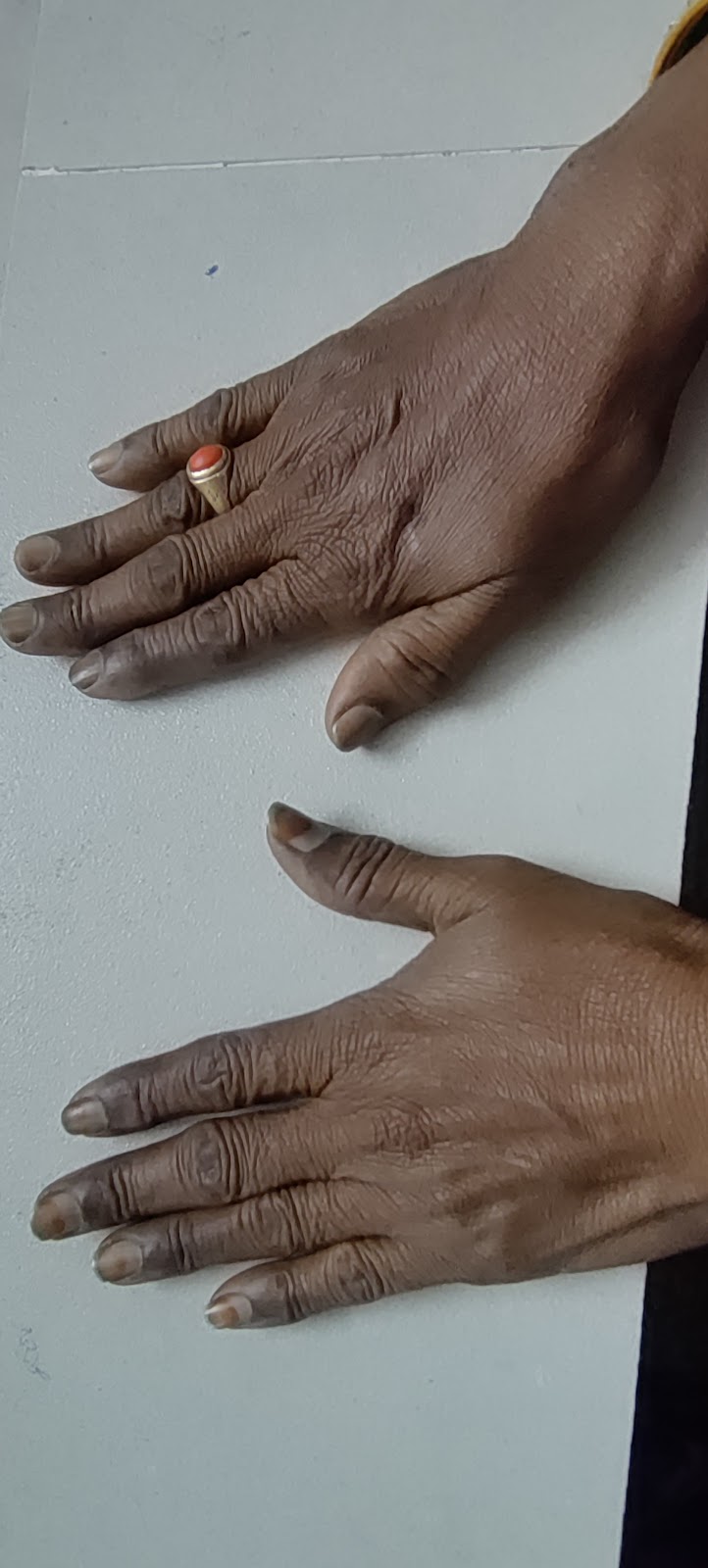
Pallor- present
Icterus-absent
Clubbing-absent
Cyanosis-absent
Generalised lymphadenopathy-absent
Pedal edema-absent
Vitals:
Temperature - 98.3F
Pulse rate - 86 bpm
Respiratory rate - 18cpm
Blood pressure -140/90mm hg
Spo2 - 98% at room air
SYSTEMIC EXAMINATION:
Cardiovascular system:
S1 and S2 heard no murmurs heard
Central nervous system:
No focal neurological deficit, cranial nerve intact
Patient is concious coherent.
Motor
Tone- normal
Power- normal
Cerebellar functions- normal
RESPIRATORY SYSTEM:
Bilateral air entry-present ,Normal vesicular breath sounds-heard
ABDOMINAL EXAMINATION:
soft and non tender, No Hepatomegaly, spleen is not palpable
RENAL FUNCTION TEST:
LIVER FUNCTION TEST
Blood sugar random




























Comments
Post a Comment