18 F DKA with perianal abscess
Chief Complaints :
A 18 Years Old Female who is a Student Presented with C/O
Pain & Swelling in Perianal Region Since 10days
Fever with Chills Since 10 Days
Shortness of Breath Since 2 Days
History of Present Illness :
Patient Was Apparently Asymptomatic 8 Years ago then She Suddenly Developed Pain Abdomen ; Shortness of Breath (grade 4) & Lethargy for Which she went to Hospital in Hyderabad & Was Diagnosed with Type 1 DM ( RBS was around 600mg/dL ) Since then She was on Inj.MIXTARD BD.
4 Years Ago She Developed Pain Abdomen Which was Sudden Onset , Diffuse , Squeezing Type ; Non Radiating & Not Relieved With Medication & Went to Hospital Where she was told it is Due to Uncontrolled Sugars & Pain Got Subsided after Treatment & Was Prescribed with Inj.MIXTARD ( 20U - Morning ; 15U - Night )
10 Days Back She Developed Swelling Around the Perianal Region Which is Initially Around 1x1cm & Gradually Progressed to Present Size Around 4x4cm,Associated with Pus Discharge with reddish skin discoloration around the swelling , Pain, Fever with Chills 5 days back which is Low Grade & Intermittent for Which She Went to Hospital 5 Days Back & Was Started on Antibiotics. After Taking These antibiotics She Started Having Nausea & Decreased Food Intake. So They Decreased the Insulin Dose to 5U Morning & 5U Night Since 3 Days. 2 Days Back She Started Having Shortness of Breath which Was Grade 2 & GRBS Was 480mg/dl for Which She Went to Local Hospital & Took Some Injections. Then after 1 Days SOB Progressed to Grade 4 & Referred to Our Hospital.
Past History :
H/O Swelling over inner Thighs associated with Pus Discharge 1 Year Ago Following 2nd Dose of COVID vaccination & Took Medication in local Hospital & Got Relived
K/C/O Type 1 DM Since 8 Years
N/K/C/O HTN ; TB ; Asthama ; Epilepsy
Personal History :
Diet : Mixed
Appetite : Decreased since 5 days
Sleep : Inadequate since 4
Bowel : not passed stools since 5 days
Bladder : regular
Addictions : Nil
Family History :
Her Father - T 2 DM Since 10 Years
GENERAL PHYSICAL EXAMINATION
Patient is conscious, coherent, coperative and well oriented to Time place and person.
She is moderately built and nourished.
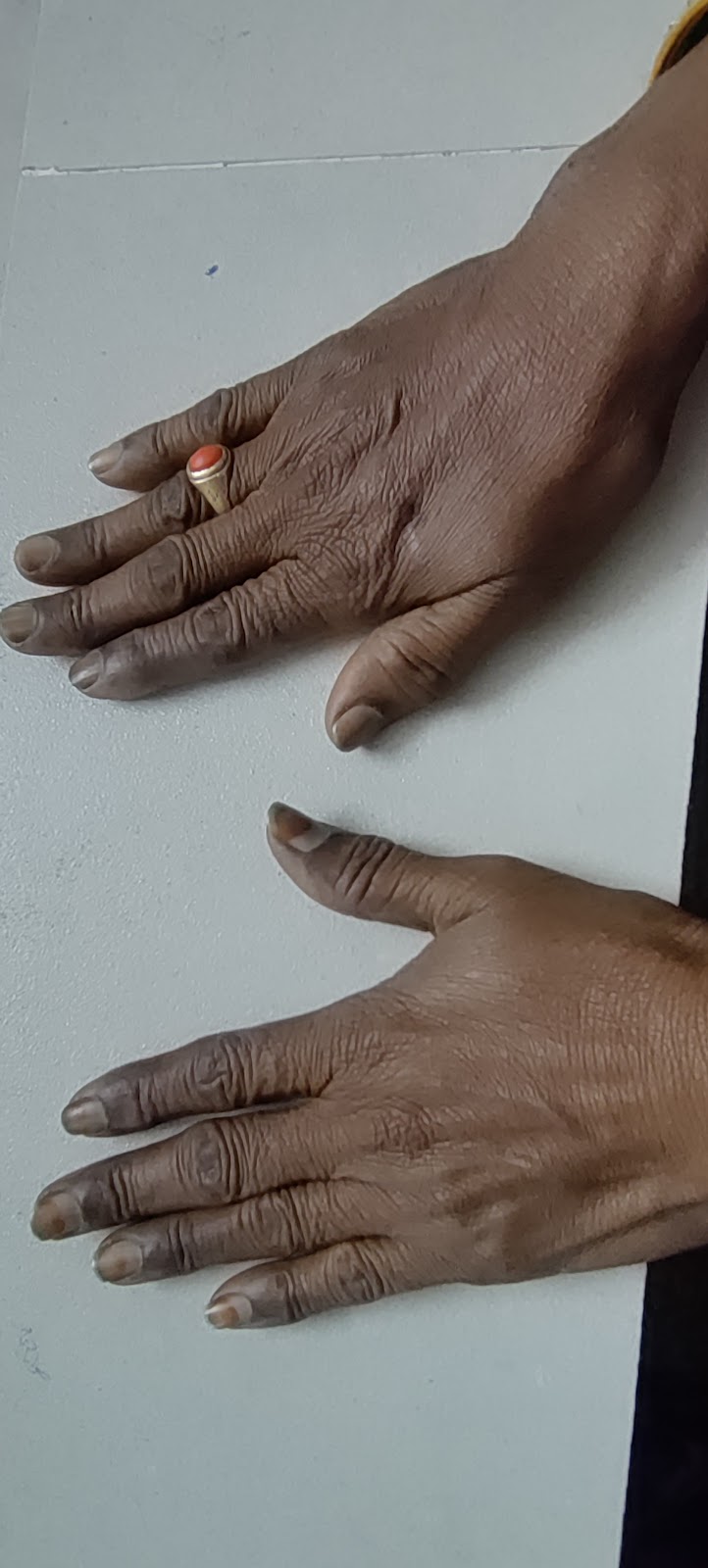
No h/ o pallor, Cyanosis, clubbing, generalized lymphadenopathy - absent.
Vitals on admission -
Temperature - 98.5F
Pulse rate - 114bpm
Respiratory rate - 28cpm
Blood pressure - 120/70mm hg
SYSTEMIC EXAMINATION
•Cardiovascular system-
S1 and S2 are heard ,no murmurs are heard.
•Respiratory system:
Trachea central, all quadrants of chest moves equally with respiration. No adventitious sounds.
Breath sounds- bilateral normal
Vesicular breath sounds are heard.
•Central nervous system-
No focal neurological deficits
•Abdominal system:
Inspection:
On inspection abdomen is flat, symmetrical.
Umbilicus is centre and inverted.
All 9 regions of abdomen are equally moving with respiration.
Palpation:
On palpation abdomen is soft and mild tender.
All inspectory findings are confirmed.
Auscultation:decreased bowel sounds






















Comments
Post a Comment