1801006143 - short case
1801006143- short case
27year old with b/l pedal edema, facial puffiness and sob
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 27 yr female patient resident of nalgonda came to opd with
chief complaints of :
-Swelling of both legs , facial puffiness since 6 days
-shortness of breath since 6 days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 10 years back then she was diagnosed with diabetes mellitus type 1 and is on insulin mitard (20u-x-16u).
she had 2 episodes of weakness, uncontrolled sugars for which she was admitted for a day &discharged ( 1st episode 5years back and 2nd episode 3 years back respectively).
on 3 months ago
patient was taken to govt hospital i/v/o sob and was diagnosed with denovo hypertension, uncontrolled sugars ( started on ? Htn medication).
One month back, she had episodes of vomitings, loose stools and was admitted in aiims & was diagnosed with pancytopenia ,diabetic nephropathy,hypertension ,vit d deficiency right eye pseduophakia and left eye imsc
6 days back she developed pedal edema and sob which was insidious in onset gradually progressive (grade 2 to 4) associated with orthopnoea and was brought to our hospital as her symptoms didn't subside.
Past history:
K/c/o dm type 1 since 10 years and is on insulin
K/c/o htn from 2 months and on t telma+clinidipine and
t metxl
H/o of right eye cataract surgery: 8 years back
Personal history:
Appetite - normal
Diet - mixed
Bowel and bladder - regular
Sleep - adequate
General examination:
Patient is conscious coherent cooperative, moderetely built and nourished.
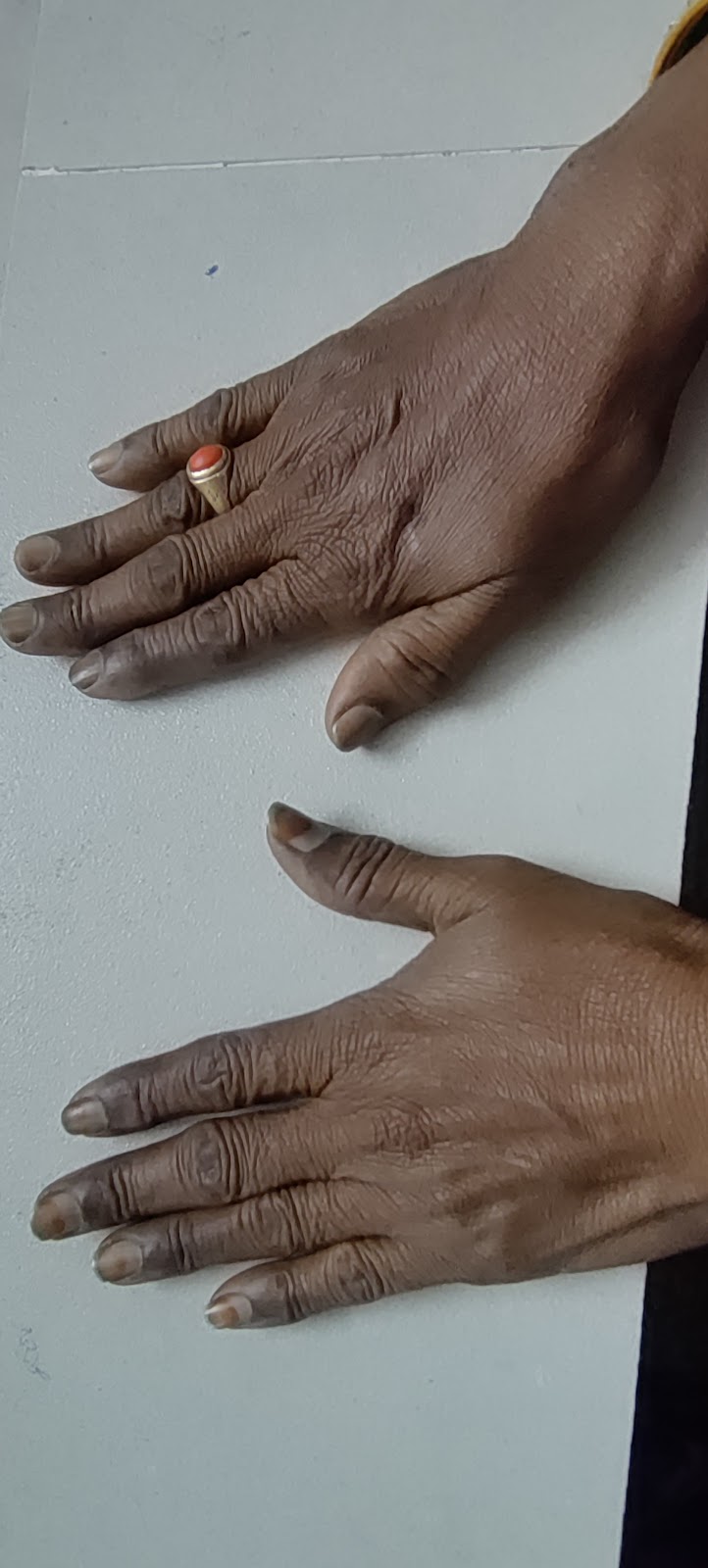
Pallor: present
Pedal edema - present,pitting type, till knee,
No icterus, cyanosis, clubbing ,Lymphadenopathy
Vitals on admission:
Pulse - 113 bpm
Bp - 220/120mm hg
Rr - 26 cpm
Spo2 - 72% at ra
Grbs - high
Systemic examination:
Per abdomen:
Inspection:
umbilicus is central and inverted, all quadrants moving equally with respiration,no scars,sinuses, engorged veins, pulsations.
Palpation: soft,non tender.no organomegaly.
Ascultation: bowel sounds - heard
Respiratory system:
*Inspection: shape of the chest is elliptical. B/l symmetrical. Both sides moving equally with respiration..no scars,sinuses, engorged veins,pulsations.
*Palpation: no local rise of temperature and tenderness.trachea is central in position.expansion of chest is symmetrical vocal fremitus is normal.
*Percussion: resonant b/l
*Ascultation: bae + , nvbs heard
CVS:
*Inspection: b/l symmetrical, both sides moving equally with respiration,no scars,sinuses, engorged veins,pulsations.
*Palpation: apex beat felt in left 5th ics
No thrills and parasternal heaves.
*Ascultation : s1 s2 + , no murmurs.
CNS:
Patient was c/c/c.
Higher mental functions- intact
Gcs - e4 v5m6
B/l pupils - normal size and reactive to light
No signs of meningeal irritation
Cranial nerves- intact
Sensory system-normal
Motor system: tone- normal
power- 5/5 in all limbs
Reflexes: biceps - 2+, triceps-2+, supinator + , knee - 2+, ankle - 2+
Diagnosis:
Type 1 diabetes mellitus with uncontrolled sugars (resolving)
With hypertensive emergency (resolved)
Bicytopenia secondary to b12 deficiency (? Nephrotic syndrome)
Investigations :
sugars were found to be high
BP - 220/110mmhg on presentation and was treated symptomatically.
Blood group: b+ve
Blood urea: 83mg/dl
Sr creatinine- 1mg / dl
HbsAg rapid- negative
LFT:
Total bilirubin- 1.47mg/dl
Direct bilirubin: 0.44mg/dl
Sgot - 39 IU/L
Sgpt -normal
ALP - 103 IU/L
Total protein: 5.6gm/dl
Albumin- 3gm/dl
TREATMENT:
1.IVF NS @ 30 ml/ hr
2.Strict diabetic diet
3.inj lasix 40 mg iv bd
4.T.telma 40 mg po bd
5.t metxl 25mg po od
6. T. Clinidipine 10 mg po bd
7.T.Nicardia 20 mg po bd
8.inj hai according to grbs
9. Inj glargine 10 u @ 10pm
10.T.Thyronorm 25mcg po od
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
A 27 yr female patient resident of nalgonda came to opd with
chief complaints of :
-Swelling of both legs , facial puffiness since 6 days
-shortness of breath since 6 days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 10 years back then she was diagnosed with diabetes mellitus type 1 and is on insulin mitard (20u-x-16u).
she had 2 episodes of weakness, uncontrolled sugars for which she was admitted for a day &discharged ( 1st episode 5years back and 2nd episode 3 years back respectively).
on 3 months ago
patient was taken to govt hospital i/v/o sob and was diagnosed with denovo hypertension, uncontrolled sugars ( started on ? Htn medication).
One month back, she had episodes of vomitings, loose stools and was admitted in aiims & was diagnosed with pancytopenia ,diabetic nephropathy,hypertension ,vit d deficiency right eye pseduophakia and left eye imsc
6 days back she developed pedal edema and sob which was insidious in onset gradually progressive (grade 2 to 4) associated with orthopnoea and was brought to our hospital as her symptoms didn't subside.
Past history:
K/c/o dm type 1 since 10 years and is on insulin
K/c/o htn from 2 months and on t telma+clinidipine and
t metxl
H/o of right eye cataract surgery: 8 years back
Personal history:
Appetite - normal
Diet - mixed
Bowel and bladder - regular
Sleep - adequate
General examination:
Patient is conscious coherent cooperative, moderetely built and nourished.
Pallor: present
Pedal edema - present,pitting type, till knee,
No icterus, cyanosis, clubbing ,Lymphadenopathy
Vitals on admission:
Pulse - 113 bpm
Bp - 220/120mm hg
Rr - 26 cpm
Spo2 - 72% at ra
Grbs - high
Systemic examination:
Per abdomen:
Inspection:
umbilicus is central and inverted, all quadrants moving equally with respiration,no scars,sinuses, engorged veins, pulsations.
Palpation: soft,non tender.no organomegaly.
Ascultation: bowel sounds - heard
Respiratory system:
*Inspection: shape of the chest is elliptical. B/l symmetrical. Both sides moving equally with respiration..no scars,sinuses, engorged veins,pulsations.
*Palpation: no local rise of temperature and tenderness.trachea is central in position.expansion of chest is symmetrical vocal fremitus is normal.
*Percussion: resonant b/l
*Ascultation: bae + , nvbs heard
CVS:
*Inspection: b/l symmetrical, both sides moving equally with respiration,no scars,sinuses, engorged veins,pulsations.
*Palpation: apex beat felt in left 5th ics
No thrills and parasternal heaves.
*Ascultation : s1 s2 + , no murmurs.
CNS:
Patient was c/c/c.
Higher mental functions- intact
Gcs - e4 v5m6
B/l pupils - normal size and reactive to light
No signs of meningeal irritation
Cranial nerves- intact
Sensory system-normal
Motor system: tone- normal
power- 5/5 in all limbs
Reflexes: biceps - 2+, triceps-2+, supinator + , knee - 2+, ankle - 2+
Diagnosis:
Type 1 diabetes mellitus with uncontrolled sugars (resolving)
With hypertensive emergency (resolved)
Bicytopenia secondary to b12 deficiency (? Nephrotic syndrome)
Investigations :
sugars were found to be high
BP - 220/110mmhg on presentation and was treated symptomatically.
Blood group: b+ve
Blood urea: 83mg/dl
Sr creatinine- 1mg / dl
HbsAg rapid- negative
LFT:
Total bilirubin- 1.47mg/dl
Direct bilirubin: 0.44mg/dl
Sgot - 39 IU/L
Sgpt -normal
ALP - 103 IU/L
Total protein: 5.6gm/dl
Albumin- 3gm/dl
TREATMENT:
1.IVF NS @ 30 ml/ hr
2.Strict diabetic diet
3.inj lasix 40 mg iv bd
4.T.telma 40 mg po bd
5.t metxl 25mg po od
6. T. Clinidipine 10 mg po bd
7.T.Nicardia 20 mg po bd
8.inj hai according to grbs
9. Inj glargine 10 u @ 10pm
10.T.Thyronorm 25mcg po od

Comments
Post a Comment