This is an a online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CHEIF COMPLAINT:
A 75 yr old male came to GM OPD with the cheif complaints of sob,fever,cough since 15 days
HOPI:
pt was apparently alright 15 days back then he developed shortness of breath (Grade II) which was insidious in onset
H/O cough not associated with sputum, aggrevated in cold weather,cool drinks
H/O fever since 2 weeks more in morning time relieved on medication
H/O headache, nausea chest pain.
H/O pain in below neck on left side (scapular- region )while lying down
No H/O palpitations, pedal edema, Abdomen distension
No H/O burning micturition
No H/O orthopnea
No H/O loss of weight
PAST HISTORY :
H/O similar complaint in past - 1 year ago
k/c/o HTN 6 yrs on T. AMLODIPINE 5 my OD
DM-II on T. METFORMIN 500mg OD
H/o TB 20yrs , 25yr and used medication
N/K/C/O Asthma, Epilepsy, CVA, CAD, thyroid disorder
FAMILY HISTORY:
No similar complaints are present in family members
PERSONAL HISTORY :
Diet: mixed
Appetite- normal
Sleep- adequate
Bladder movements- Regular
Bowel movements- Regular
GENERAL EXAMINATION AT ADMISSION
Patient is conscious, coherent and cooperative. Well oriented to time,place and person,well built and nourished
Pallor-absent
Icterus-absent
Cyanosis-absent
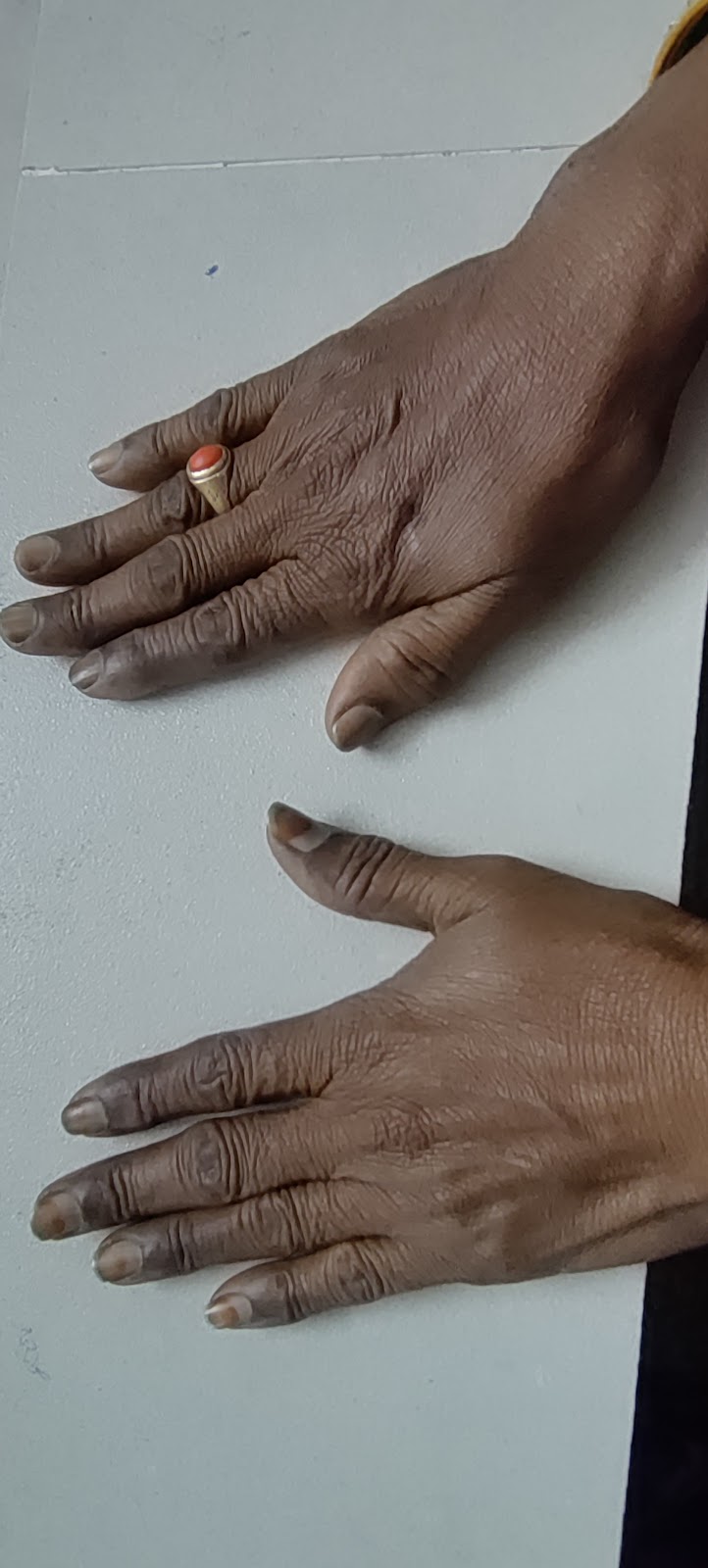
Clubbing-absent
Lymphadenopathy -absent
Edema-absent
VITALS ON ADMISSION
BP -120/70mmhg
PR-72bpm
RR- 20cpm
TEMP- Afebrile
SPO2- 100 @room air
GRBS-102mg/dl
SYSTEMIC EXAMINATION
R/S -
INSPECTION
Position of trachea-central
shape of chest - Elliptical
chest -Asymmetrical
TACTILE FREMITUS - R.L.
Increased on right side compared to left side
PERCUSSION - R.L.
-dullness on rt side compared to left side
Auscultation:
Crackles heard on left side
Normal sounds on left side
CVS:s1, s2 heard ,no murmurs.
P/A : Soft, non tender, no organomegaly
CNS:
Higher motor functions - intact
Cranial nerves - intact
Motor system:
Rt- UL. LL. Lt- UL. LL
Bulk - N N. N. N
Tone - N. N. N. N
Power - 5/5. 5/5. 5/5. 5/5
Reflexes:
UL LL
Biceps. 2+. 2+
Triceps. 2+. 2+
Supinator. 2+. 2+
Knee. 2+. 2+
Ankle. 2+. 2+
Sensory system: intact
Co ordination is present
✓DROOPING OF RIGHT SHOULDER
INVESTIGATIONS:
Random blood sugar-101 mg/dl
Glycated hemoglobin- 6.5%
Fasting blood sugar-96 mg/dl
Hemogram-
RFT-
LFT-
CUE-
Chest X ray (PA view) -
HR CT lung video link:
1.
https://youtube.com/shorts/T9JRuNxpiec?si=rd5ecbgaDoCtPUry
2.
https://youtu.be/IP8dgUMNX_A?si=1ugsnUFM8jEABeVh












Comments
Post a Comment