67 Y/ M CAME WITH C/O CHEST PAIN SINCE 3 DAYS C/O NECK PAIN SINCE 3 MONTHS
C/O CHEST PAIN SINCE 3 DAYS
C/O NECK PAIN SINCE 3 MONTHS
HOPI:
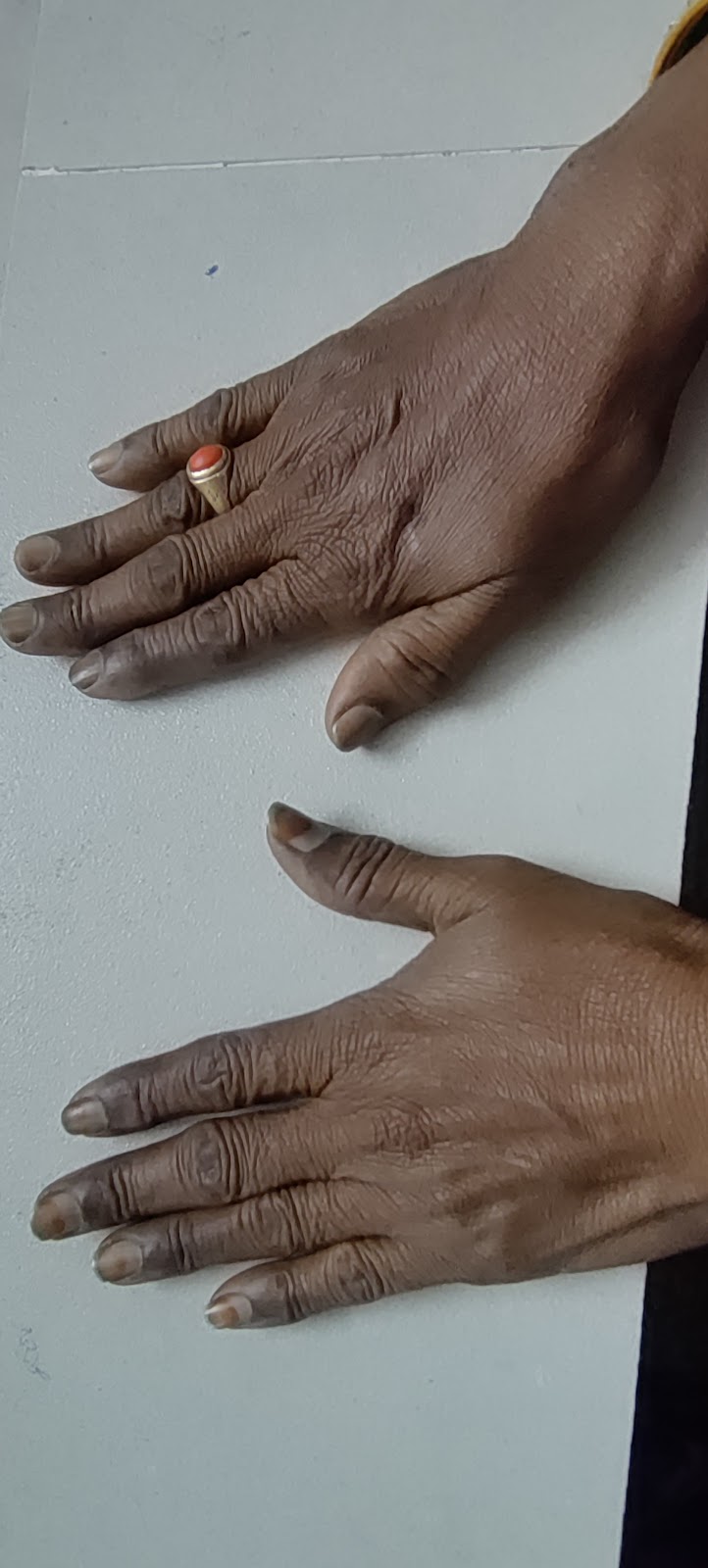
PATIENT WAS APPARENTLY ASYMPTOMATIC 3 MONTHS BACK THEN DEVELOPED NECK PAIN INSIDIOUS IN ONSET DRAGGING TYPE RADIATING TO SHOULDER A/W GIDDINESS, TINGLING AND NUMBNESS OF UPPER LIMBS
CHEST PAIN INSIDIOUS ONSET NO AGGRAVATING FACTORS, RELIEVED ON MEDICATION A/W BREATHLESSNESS
H/O ABDOMINAL PAIN, RT LOIN PAIN
H/O BURNING MICTURITION
H/O BELCHING AND BLOATING
NO H/O FEVER, PALPITATIONS AND PEDAL EDEMA
NO H/O FACIAL PUFFINESS
PAST HISTORY
H/O SURGERY FOR RENAL STONES 2 TIMES IN RIGHT KIDNEY 7 YRS BACK
H/O SURGERY FOR CATARACT BOTH EYES 4 YRS BACK
K/C/O DM II SINCE 3 YEARS GLIMI M1 PO OD
N/K/C/O HTN, CVA, CAD, THYROID DISEASE ND EPILEPSY, TB
PERSONAL HISTORY:
DIET:MIXED
SLEEP:ADEQUATE
BOWEL AND BLADDER:REGULAR , BURNING MICTURATION
ADDICTIONS: ALCOHOL 90 ML TWICE A WEEK FOR 20 YRS
APPETITE:NORMAL
GENERAL EXAMINATION:
PATIENT IS CONSCIOUS,COHERENT,COOPERATIVE,WELL ORIENTED TO TIME,PLACE AND PERSON.
NO PALLOR,ICTERUS CYANOSIS,CLUBING,LYMPHADENOPATHY,EDEMA.
VITALS:
TEMPERATURE:98.6
BP:130/70 MM HG
PR:80 BPM
RR:18 CPM
SYSTEMIC EXAMINATION:
CVS:S1,S2 HEARD NO MURMURS.
RS:BAE +,NO MURMURS
PER ABDOMEN:SOFT,NON TENDER,NO ORGANOMEGALY
CNS:NO FOCAL NEUROLOGICAL DEFICITS.
UROLOGY REFERRAL DONE ON 29/1/24 I/V/O B/L RENAL CALCULI AND LEFT RENAL CYST.
ADVICE: TAB PCM 650 MG PO BD
SYP ALKASTONE PO BD 15 ML IN HALF GLASS WATER FOR 3 MONTHS
INVESTIGATIONS:
HBsAg-RAPID 27-01-2024 04:26:PM Negative
Anti HCV Antibodies - RAPID 27-01-2024 04:26:PM Non Reactive
COMPLETE URINE EXAMINATION (CUE) 27-01-2024 04:26:PM
COLOUR Pale yellow
APPEARANCE Clear
REACTION Acidic
SP.GRAVITY 1.010
ALBUMIN Nil
SUGAR Nil
BILE SALTS Nil
BILE PIGMENTS Nil
PUS CELLS 2-3
EPITHELIAL CELLS 2-3
RED BLOOD CELLS Nil
CRYSTALS Nil
CASTS Nil
AMORPHOUS DEPOSITS Absent
OTHERS Nil
RFT 27-01-2024 04:26:PM
UREA 15 mg/dl 50-17 mg/dl
CREATININE 1.2 mg/dl 1.3-0.8 mg/dl
URIC ACID 5.0 mg/dl 7.2-3.5 mg/dl
CALCIUM 9.9 mg/dl 10.2-8.6 mg/dl
PHOSPHOROUS 2.8 mg/dl 4.5-2.5 mg/dl
SODIUM 137 mEq/L 145-136 mEq/L
POTASSIUM 3.6 mEq/L 5.1-3.5 mEq/L
CHLORIDE 99 mEq/L 98-107 mEq/L
LIVER FUNCTION TEST (LFT) 27-01-2024 04:26:PM
Total Bilurubin 0.75 mg/dl 1-0 mg/dl
Direct Bilurubin 0.14 mg/dl 0.2-0.0 mg/dl
SGOT(AST) 15 IU/L 35-0 IU/L
SGPT(ALT) 15 IU/L 45-0 IU/L
ALKALINE PHOSPHATE 203 IU/L 119-56 IU/L
TOTAL PROTEINS 6.4 gm/dl 8.3-6.4 gm/dl
ALBUMIN 4.22 gm/dl 4.6-3.2 gm/dl
A/G RATIO 1.99
POST LUNCH BLOOD SUGAR 27-01-2024 04:28:PM 249 mg/dl 140-0 mg/dl
HBA1C - 6.8
FBS 137 MG/DL
HB - 14 GM/DL
TLC - 7200
PTL- 2.06
USG DONE ON 29/1/24
FINDINGS:
E/O FEW CALCULI, LARGEST 4-5MM IN MID POLE AND LOWER POLE OF RIGHT KIDNEY
E/O 13 X 12 MM CYST NOTED IN MID POLE OF LEFT KIDNEY
E/O FEW CALCULI , LARGEST 2-3MM IN LEFT KIDNEY.
IMPRESSION : B/L RENAL CALCULI
LEFT RENAL CYST
DIAGNOSIS:
ACID PEPTIC DISEASE
DIABETES MELLITUS
CERVICAL SPONDYLOSIS
TAB GLIMI M1 1--0--0 CONTINUE
TAB PAN OD 1--0--0 BEFORE BREAK FAST FOR 5 DAYS
SYP SUCRALFATE 10 ML TID 1--1--1
TAB ULTRACET 1--0--1 FOR 5 DAYS
TAB. BENFOMET PLUS PO/OD 0--1--0 FOR DAYS
TAB SHELCAL 0--1--0 FOR 15 DAYS
TAB PCM 650 MG PO BD FOR 5 DAYS 1--0--1
SYP ALKASTONE 15 ML IN HALF GLASS WATER PO BD FOR 3 MONTHS 1--0--0
AVOID SPICY FOOD
COMPLETE ABSTINENCE OF ALCOHOL




Comments
Post a Comment